Value-Based Care Quality Metric Overload?
April 5, 2024

Build a cross-functional measurement system to manage payer programs for real ROI impact
Quality measurement programs have become critical for healthcare providers shifting further from fee-for-service (FFS) to value-based care (VBC) models. Change always brings challenges, and VBC is no different. But ask healthcare executives about their quality measurement programs, and you may find the main challenge isn’t about quality, but quantity. How can they transform voluminous amounts of disparate quality data into a meaningful improvement in value?
Between requirements for Medicare Stars, HEDIS (Healthcare Effectiveness Data and Information Set), and other payer-specific risk arrangements, the sea of VBC quality data and metrics leaves many healthcare providers adrift. It can be a tall order for hospital systems to synthesize and prioritize hundreds of different quality metrics across dozens of VBC contracts and use the results to chart a course to profitability, all while limiting disruptions to providers, patients, and administrative staff.
We will explain how to chart that course. But first, we take a closer look at the VBC “metrics overload” struggle, which can be boiled down to three key challenges:
- Lack of Standardization: The quality metrics in different VBC programs are often intended to measure very similar things, but they use different benchmarks and scoring methodologies across different populations. At the metric level, this can quickly multiply into a plethora of data that sows confusion. Providers engaged in several VBC program contracts will regularly confront the following hurdles:
- Similar quality metrics are applied to different populations for different payers with different benchmarks and calculation methodologies.
- Multiple data sources are needed to collect the quality metrics.
- Different time periods are used for measuring quality and financial impact.
- There are different requirements for commercial and government programs (Medicare and Medicaid), as well as ACOs, with different standards and calculation methods.
- Complexity of Measurement Systems: With varying point systems, percentage schedules, and benchmark scaling using sophisticated actuarial adjustments, the complexity of measurement systems makes it more difficult to put program and contract metrics on an apples-to-apples basis and track and audit them effectively. Providers are often left submitting data to payers with no ability to calculate or audit final results, and so have little choice but to accept whatever final reports payers give them at year end. Measurement complexity also makes it hard for providers to identify areas for improvement, both clinically and financially.
- Clinical and Financial Disconnect: Many health systems excel at measuring clinical performance OR financial results separately (especially in the FFS realm). However, most struggle to connect clinical performance and contracts’ financial results in a way that drives performance outcomes, which is what’s necessary in order to effectively inform decision-making and maximize value. This disconnect between financial and clinical tracking at the individual metric level makes it difficult to align priorities between the CMO and CFO.
Avoiding Expensive Mistakes
To address these hurdles, many healthcare organizations rush to assume either a “technology” mindset or a “quality” mindset, which often involves investment in expensive technology solutions or comprehensive quality improvement initiatives. Most organizations are not equipped to manage the hurdles using their current analytic and data aggregation structure, so they invest enormously in either new technology or process changes.
The problem is that most current technology and quality improvement programs do not specifically link financial contracts and clinical quality together, let alone align providers’ performance goals with multiple payers’ quality program requirements. The result is that they can lead to frustration, unachieved objectives, and the belief that investing in them was a waste of time and money. Luckily, there is a solution.
Data Validity and Alignment Drive Outcomes
The solution lies in measuring and tracking quality and value accurately, as well as in better connecting clinical and financial outcomes. This in turn requires ensuring data validity. The place to start is to evaluate an organization’s existing value-based programs and payer quality management processes. This evaluation should include a careful review and assessment of each quality program provision and contract term, as well as payer report cards with clinical and financial results.
Along with ensuring data validity, it is also vital to ensure organizational alignment. Key stakeholders across relevant disciplines should be given an opportunity to participate in a conversation about how best to connect and advance clinical quality, financial health, and improved patient outcomes. An interdisciplinary approach of this kind requires bringing together individuals with expertise in contracting, clinical improvement, and actuarial analysis to work together toward a common goal. Using this approach, health systems have had success in standardizing, simplifying, and improving payer quality programs.
Putting It All Together
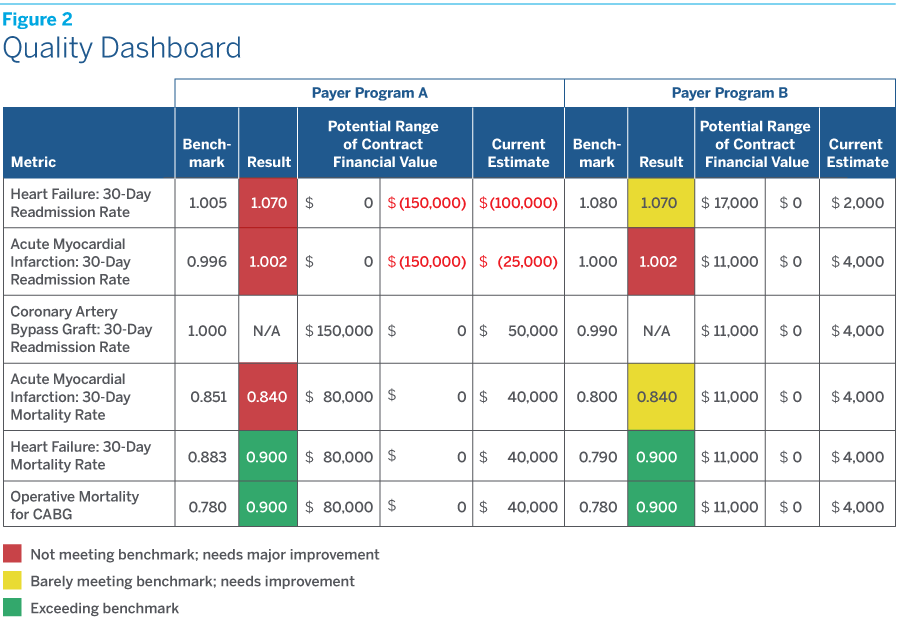
To support such an effort, a tool is needed that helps healthcare leaders visualize how financial outcomes are linked to clinical performance, and thus allows them to prioritize actionable changes in clinical operations. Transforming the morass of information extracted from a database into a quality dashboard can give leaders the clarity and comparability they are looking for to break down silos and take meaningful action.
To help contracting and clinical teams prioritize the most important metrics across programs, an effective quality dashboard should include:
- Quality metrics comparison across all payers’ programs (both government and commercial) to enable effective analysis.
- Financial values (upside and downside potential) using an actuarially sound methodology.
- Clinical values, including both the program’s benchmark and actual result, for each metric.
- Other valuable clinical information, such as service line and care-setting categories, to give clinical leaders more actionable data for further performance improvement efforts.
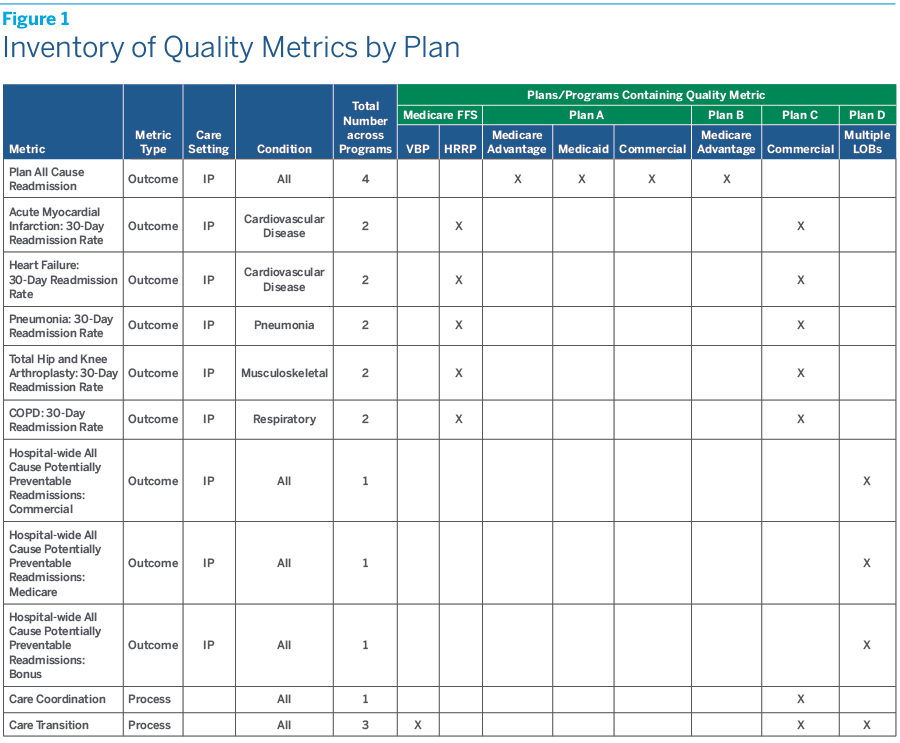
The first step is to develop a consolidated inventory that catalogs the entire universe of payer quality metrics across all VBC programs. This will not only clarify what metrics exist organization-wide, but will also help in reviewing and prioritizing them.
Figure 1 shows a simplified example of an inventory of quality metrics across multiple payer programs.
Figure 2 shows a simplified example of a quality dashboard indicating the financial risk (range of financial outcomes) associated with the various quality metrics.
Using the Dashboard for Maximum Impact
The quality management process and quality dashboard can supercharge your VBC program success in a variety of ways, and ultimately inform more productive partnerships between payers and providers. The dashboard has been adopted and used by several health systems with great success. Here are just a few uses reported back from those health systems to consider:
- Inventory payer quality metrics and prioritize them to identify high-value metrics that represent, for instance, 80% of the financial value of your VBC programs and have meaningful clinical impacts for your health system. You can then easily track and monitor this data through the quality dashboard. In some payer contracts, metrics may be grouped together, requiring the provider to meet targets for all metrics, but it can nonetheless be helpful to assign a portion of financial risk to individual metrics to get an understanding of the magnitude of risk for a given metric across payers.
- Help leadership set improvement goals and develop strategies for ROI results at the beginning of the year.
- Improve quality performance for CMS programs by looking closely at your organization’s performance across all payers and lines of business. CMS Value-Based Purchasing (VBP) programs are penalty programs with significant dollar impacts. A quality dashboard enables users to compare CMS programs with commercial programs to identify pain points that can be improved across the organization, instead of focusing on results in a silo.
- Negotiate with commercial payers to either reduce quality metrics or replace them with more meaningful metrics that positively affect outcomes. A quality dashboard enables users to prioritize metrics financially and clinically to identify “core high-value metrics.” Providers can use these to negotiate with partner payers to either reduce quality metric numbers or choose more standardized and meaningful metrics that really matter.
- Request actionable data and reports from payers to support clinical improvement. Don’t settle for standard reporting that may not provide relevant or insightful information. Ask for data based on what you are seeing in your dashboard and, if necessary, request new metrics that can better inform your decision-making for continued success.
- Encourage an interdisciplinary decision-making process that involves both the contracting department and clinical team to prioritize and track metrics based on both financial impact and clinical importance.
A Common Vision in High-Value Care
The VBC quality management process and quality database/dashboard we have described can be adopted broadly by any healthcare organization to solve the challenges with VBC payer arrangements that many leadership teams face today. It can help contracting departments and frontline clinicians improve both financial and clinical performance and achieve a high-value care vision—delivering value in both quality and cost.
The right partner can help providers take full advantage of their VBC arrangements. Contact us at info@terrygroup.com to learn more about how Terry Health applies its process management, data science, compliance, and change management expertise to help organizations thrive in today’s evolving healthcare ecosystem.